DUBAI: Mental-health campaigners in the Middle East say it is high time for teachers, parents and policymakers to encourage young people to open up about their feelings and break free from the shame surrounding discussion of psychological disorders.
The warning comes after two separate surveys highlighted the scale of suffering among the region’s 200 million Arab youth due to depression, anxiety and addiction.
The Arab Youth Survey 2019, released earlier this month by the Dubai-based communications company Asda’a BCW, showed mental illness to be a widespread concern among young people in the Middle East and North Africa (MENA). And a recent YouGov poll conducted in the UAE pointed to the existence of a stigma around mental illness, with fewer than half of respondents saying they would seek professional help if they were suffering from a psychological disorder.
“The Arab population is plagued by issues that are no different from any other population in the world: Depression, anxiety, eating disorders, addiction, suicide, self-mutilation, post-traumatic disorders, mood disorders and so on,” Fadwa Lkorchy, a psychologist at the Dubai-based German Neuroscience Center, told Arab News. “The difference now is that the Arab world is willing to admit the problem.”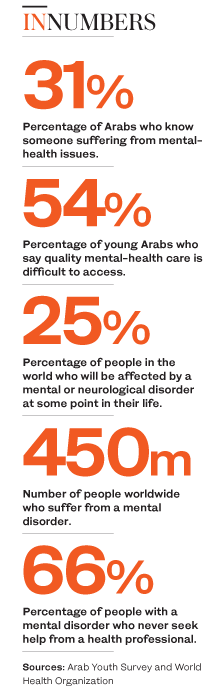
The Arab Youth Survey, which explored attitudes among Arab youth in 15 countries and territories in MENA, found that one-third of them knew someone suffering from a mental disorder such as anxiety and depression.
Half of the respondents — Arab men and women aged 18 to 24 — said there was a stigma attached to seeking medical care.
Youth in the Gulf Cooperation Council (GCC) countries are most likely to be accepting of mental illness, according to the Arab Youth Survey, with 62 percent saying it was a normal thing.
GCC youth identified personal relationships as the biggest source of stress, followed closely by academic factors.
“The young generations are more exposed than the older ones to what’s going on around the world,” said Lkorchy.
“They have higher expectations but not the same resilience, which may result in feelings of inadequacy in matters of education, career and lifestyle,” she added.
“Now is the right time to talk about mental illness, to help people deal with daily challenges and develop skills to improve their mental wellbeing.”
Lkorchy said the polls’ findings point to at least two things: Young people should not delay seeking medical care for underlying psychiatric disorders, and medical professionals need to provide better and a wider range of platforms for young people to discuss mental-health issues or receive treatment. “The mental-health statistics aren’t surprising. We’ve seen for decades the neglect of mental health and focus solely on physical health,” she added. “The new generations, with help from social media, are more open and willing to seek help.”
Dr. Justin Thomas, professor of psychology at Zayed University in Abu Dhabi and author of “Psychological Wellbeing in the Gulf States,” told Arab News that the new focus of this year’s Arab Youth Survey on mental health is timely because disorders, despite being widely underreported, have reached “epidemic proportions in many nations.”
Stigmatization of people with mental illness is “very real, and in spite of the many brave celebrity self-disclosures, it persists and will undoubtedly continue to endure for generations to come,” Thomas said.
“While most nations no longer attempt to exterminate or sterilize people with mental-health issues, we do continue to shun, stigmatize, demonize and discriminate,” he added.
“People will often exclude or ridicule individuals known to have experienced mental-health issues.”
Lkorchy said although a number of clinics in the UAE and Saudi Arabia now offer mental-health care, the high cost is often a deterrent to using their services.
“All medical insurance should include mental-health services, not only for treatment but also for prevention,” she added.
“Mental illness can lead to psychosomatic disorders and autoimmune diseases, of which we are seeing more cases of late.”
One of the biggest obstacles to addressing psychological disorders in MENA is the stigma surrounding the topic.

Iraqi boys attend a class at a school in west Mosul on July 27, 2017. (AFP)
Dr. Shaju George, a specialist in psychiatry at Al Zahra Hospital in Sharjah, the UAE, told Arab News: “Ignorance, lack of motivation, non-availability of facilities and properly trained professionals, lack of government funding and insurance coverage — each of these could be playing a role.”
He said: “Unidentified and untreated psychiatric disorders of tomorrow’s citizens could affect the future of the country as a whole.” He added: “If underlying mental-health issues go unnoticed, the results could affect young people’s scholastic achievements, work performance and ultimately their careers.”
Of the 1,085 participants in the YouGov poll, 72 percent said they would seek — or suggest seeking — help from a mental-health professional if they, or a person they are close to, were struggling with an issue.
A majority would look for expert assistance for issues such as suicidal thoughts (62 percent), self-harm (61 percent), hallucinations or delusions (56 percent), anxiety (55 percent) and post-traumatic stress disorder (53 percent).
Since mental health is a taboo topic for many, “increasing awareness is the key,” said George. “Imparting the right knowledge and instilling hope can assist in removing the stigma, which in turn will prompt more people to seek professional mental-health care. We can see great initiatives in this area in the GCC.”
The importance of more research and data to ascertain the scale of the Middle East’s mental-health challenge in order to dedicate adequate resources cannot be overstated, he added.
A 2017 study titled “Predictors of adolescents’ mental health problems in Saudi Arabia” examined feedback from 12,121 students and found a strong correlation between “poor relationship with parents, negative body image, and chronic illness” and worry, sadness and hopelessness.
The study’s authors said: “Symptoms suggestive of mental health problems among adolescents in Saudi Arabia are prevalent and deserve special attention.”
They recommended that “annual screening for depression ... should be implemented in schools. Effective professional counseling services should be implemented at all schools to help … students better cope with their problems.”
George said mental illness should be understood and treated as a medical or physiological disorder, rather than as an abstract condition.
“This alone will bring about a major change in the attitudes of people and their readiness to seek medical care,” he added.
“This idea needs to be introduced into school and college curricula, discussed at gatherings by religious heads, incorporated into government-funded mental-health programs and community outreach events, and adopted by media to raise public awareness.”
Health is a state of complete physical and mental wellbeing as defined by the World Health Organization, George said, “therefore good physical health means good mental health, and vice versa.”












